Could the vibrant strokes of a masterpiece, the raw emotion etched onto a canvas, be a window into the turmoil of the human mind? The life and art of Edvard Munch, particularly his iconic "Idealization," suggest a compelling connection to Borderline Personality Disorder (BPD), a mental health condition characterized by emotional dysregulation.
The enigmatic world of mental health often intertwines with the creative realm, leaving us to ponder the relationship between the artist and their work. In the case of Edvard Munch, the Norwegian painter whose expressionist style captured the essence of human suffering, the shadow of BPD looms large. His work, particularly "Idealization" from 1903, exhibits the raw, unfiltered emotions often associated with this complex disorder. The swirling colors, distorted figures, and palpable sense of unease reflect the internal chaos that those with BPD often experience. The painting offers a glimpse into the psychological landscape marked by unstable relationships, a distorted sense of self, and intense emotional fluctuationshallmarks of the condition. The artist's own life, marked by personal tragedies and tumultuous relationships, further fuels the speculation. The diagnosis, while not definitively confirmed during his lifetime, allows for a deeper understanding of Munch's artistic vision, and can also help give context to his overall life.
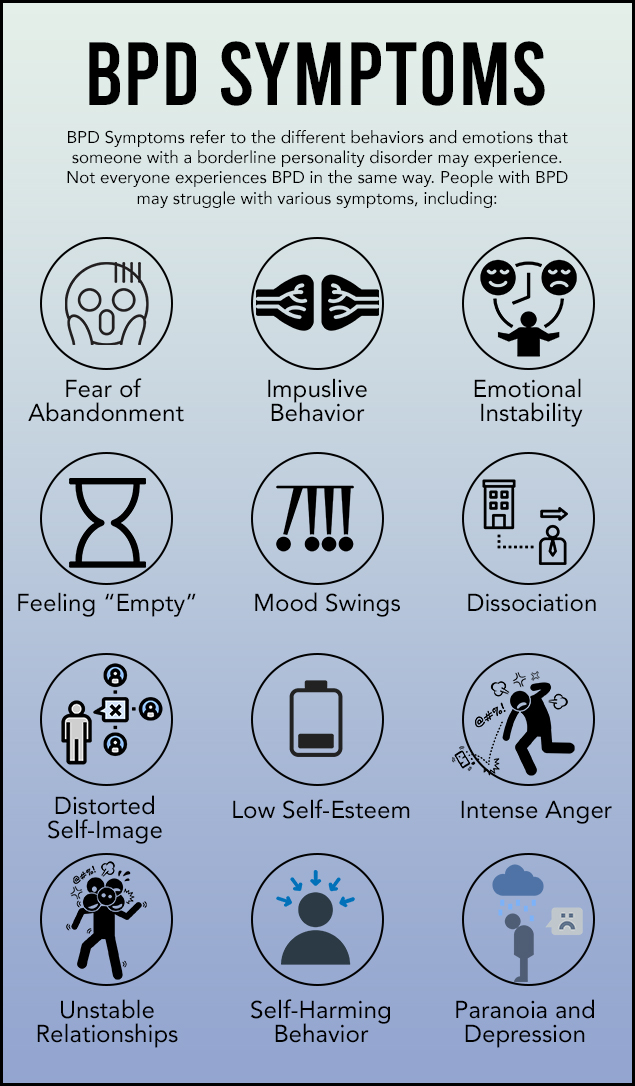
Borderline Personality Disorder is a mental illness that severely impacts a persons ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others. Early recognition of borderline personality disorder symptoms and signs can be important for coping with the condition. However, there are certain signs and symptoms that can indicate borderline personality disorder may be present. The disorder is marked by unstable moods, behaviors, and relationships. These symptoms often result in impulsive actions and problems in relationships with others. People with BPD experience wide mood swings and can feel a great sense of instability and insecurity. BPD is a mental health condition that affects the way you feel about yourself and other people. The symptoms often start during the teen years. Symptoms can be a bit different for each person. But people with BPD will have at least five of these symptoms over time. These include: efforts to avoid real or imagined abandonment, intense bouts of anger, depression, or anxiety, extreme anger and problems controlling anger.
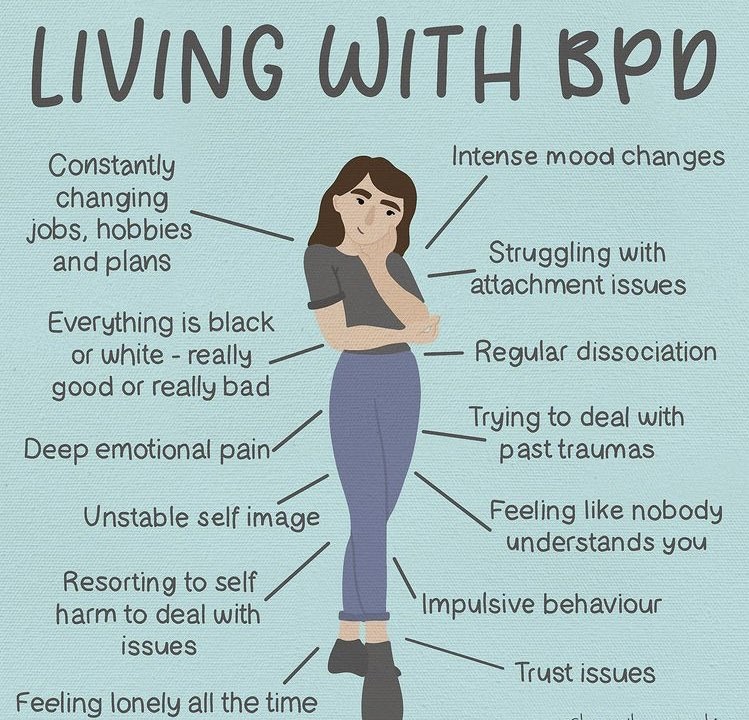
The journey through BPD is often marked by a complex interplay of internal and external factors. The common symptoms, which can vary in intensity and manifestation from individual to individual, often cluster around four main areas: emotional instability, cognitive distortions, interpersonal difficulties, and behavioral dysregulation. Emotional dysregulation, the cornerstone of BPD, manifests as intense and fluctuating moods. The individual might swing rapidly between extremes of joy, sadness, anger, or anxiety, often triggered by seemingly minor events. These mood swings can last for hours or days, leaving the person feeling overwhelmed and out of control. The fear of abandonment, whether real or imagined, fuels many of the interpersonal challenges. Individuals with BPD often crave intimacy but struggle to maintain healthy relationships. They may idealize others initially, only to quickly devalue them when they perceive a slight or feel rejected. This pattern can lead to a cycle of tumultuous relationships, characterized by emotional intensity, conflict, and instability. Impulsivity, another hallmark of BPD, can manifest in various ways, including reckless spending, substance abuse, unsafe sexual behaviors, or reckless driving. These impulsive actions are often attempts to cope with overwhelming emotions or to fill an inner void. Cognitive distortions, such as black-and-white thinking (seeing things as either all good or all bad), can further complicate the experience of BPD. These distortions can lead to misinterpretations of events and contribute to relationship problems. The persons self-image is often unstable and negative, leading to feelings of worthlessness, emptiness, and a lack of identity.
Borderline Personality Disorder (BPD) can cause a wide range of symptoms. These symptoms can be broadly grouped into four main areas. Learning about borderline personality symptoms, causes, and treatments is crucial for effective management. The symptoms often result in impulsive actions and problems in relationships with others. Finding resources on the signs and symptoms of borderline personality disorder and potential treatments and therapies is essential. People with BPD experience wide mood swings and can feel a great sense of instability and insecurity. What are the symptoms of borderline personality disorder? Symptoms can be a bit different for each person. But people with BPD will have at least five of these symptoms over time.
Borderline Personality Disorder is usually diagnosed in late adolescence or early adulthood. Occasionally, a person younger than age 18 may be diagnosed with BPD if symptoms are significant and last at least a year. BPD can be difficult to diagnose, as many of its symptoms can be mistaken for signs of a mood or identity disorder. Symptoms of BPD usually begin in late adolescence or early adulthood. BPD is more commonly diagnosed in women (about 75% of cases) than men. There are treatment options for BPD that can lessen symptoms and improve your quality of life. In addition, studies show that the overall rate of remission (improvement of symptoms) among people treated for BPD can be high, and symptoms can improve with time. The types and severity of BPD symptoms may differ from person to person because people have different predispositions and life histories, and symptoms can fluctuate over time.
All personality disorders are lifelong patterns, but there is now more optimism about the more distressing aspects of BPD. Research indicates that the symptoms of BPD get less intense as people grow older. BPD is a mental health condition that can make it hard to regulate strong emotions. People with BPD may experience symptoms including impulsivity, difficulty. The symptoms of BPD can be grouped into 4 main areas. Learn about the signs and symptoms of borderline personality disorder, a mental health condition that affects how you feel about yourself and others. Find out the possible causes, risk factors, complications, and treatment options for this disorder. Learn about the common symptoms of borderline personality disorder (BPD), such as fear of abandonment, unstable relationships, and emotional instability. Find out how to get a diagnosis and treatment for BPD, and how it can improve over time. BPD is a mental health condition marked by extreme mood swings, unstable relationships, and impulsive behavior. Learn about the signs, causes, and treatment options for BPD from Cleveland Clinic. Find out the possible causes, how BPD is diagnosed, and what treatments are available. Learn about the nine traits of BPD, a mental health condition that affects how you think, feel, and behave. Find out how to recognize, cope with, and treat BPD with effective strategies and support. Learn about the common signs of BPD, such as fear of abandonment, mood swings, impulsive behavior, and disturbed thinking. Find out how BPD affects relationships, triggers, and how it differs from bipolar disorder.
The challenges of BPD extend beyond the individual, impacting their relationships with family, friends, and romantic partners. The intense emotions, fear of abandonment, and impulsive behaviors can create a volatile environment. Loved ones may struggle to understand the fluctuating moods and unpredictable actions, leading to feelings of frustration, exhaustion, and even resentment. Communication can break down, trust can erode, and relationships can become strained. Yet, its important to remember that the individual with BPD is not intentionally trying to cause harm. Their behavior is often a manifestation of their internal struggles, and they may be deeply remorseful for the pain they inflict on others. Building and maintaining healthy relationships requires empathy, understanding, and a willingness to learn about the condition. Open communication, clear boundaries, and professional support can help both the individual with BPD and their loved ones navigate the challenges and foster a more supportive environment.
The diagnosis of BPD usually takes place in late adolescence or early adulthood, the onset of symptoms often occurring during the teen years. However, the disorder can be difficult to diagnose, as many of its symptoms overlap with other mental health conditions, such as depression, bipolar disorder, and post-traumatic stress disorder (PTSD). Furthermore, individuals with BPD may be reluctant to seek help due to feelings of shame, stigma, or distrust. A proper diagnosis requires a comprehensive evaluation by a qualified mental health professional, which may include a clinical interview, psychological testing, and a review of the individual's history. The clinician will assess the presence of at least five of the nine diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These criteria include the previously mentioned hallmarks of BPD: emotional instability, fear of abandonment, unstable relationships, impulsivity, suicidal or self-harming behaviors, feelings of emptiness, inappropriate anger, transient paranoid ideation, or severe dissociative symptoms. It is crucial to seek professional help for an accurate diagnosis and to rule out any co-occurring conditions, as BPD often coexists with other mental health disorders, such as depression, anxiety disorders, eating disorders, and substance use disorders.
Treatment for BPD is multifaceted and typically involves a combination of psychotherapy, medication, and lifestyle modifications. Psychotherapy, or talk therapy, is considered the cornerstone of treatment, as it provides individuals with the skills and tools to manage their emotions, behaviors, and relationships. Dialectical Behavior Therapy (DBT) is a particularly effective form of therapy for BPD, as it focuses on developing mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness skills. Other types of therapy, such as Cognitive Behavioral Therapy (CBT) and psychodynamic therapy, may also be beneficial. Medication may be prescribed to address specific symptoms, such as mood swings, anxiety, or depression. While there is no single medication that specifically treats BPD, antidepressants, mood stabilizers, and anti-anxiety medications can help to manage the associated symptoms. Lifestyle modifications, such as regular exercise, a healthy diet, sufficient sleep, and stress-reduction techniques, can also play a significant role in managing the symptoms of BPD and improving overall well-being. Support groups and peer support can also provide valuable resources and a sense of community for those living with BPD.
The prognosis for BPD is generally favorable, with many individuals experiencing significant improvement in their symptoms over time. Research indicates that the symptoms of BPD tend to diminish in intensity with age, and many individuals achieve remission, meaning they no longer meet the diagnostic criteria for the disorder. The duration and severity of BPD symptoms can vary widely from person to person, and factors such as access to treatment, the severity of symptoms, and the presence of co-occurring conditions can influence the course of the disorder. However, with proper treatment and support, individuals with BPD can learn to manage their symptoms, build healthy relationships, and lead fulfilling lives. The focus of treatment is not to cure BPD, as it is a personality disorder, but to provide individuals with the tools and strategies they need to cope with their emotions, improve their behaviors, and live a life that is more stable and meaningful. Regular therapy sessions, ongoing medication management (if applicable), and self-care practices are essential for maintaining progress and preventing relapse. Resilience, the ability to bounce back from adversity, is a key factor in the long-term well-being of individuals with BPD.